Medicaid and CHIP Coverage
Medicaid and the Children’s Health Insurance Program (CHIP) provide free or low-cost health coverage to millions of Americans, including some low-income people, families and children, pregnant women, the elderly, and people with disabilities. Some states have expanded their Medicaid programs to cover all people below certain income levels. Medicaid & CHIP program names vary, so make sure to find out what they’re called in your state.
Even if you don’t qualify for Medicaid based on income, you should apply. You may qualify for your state’s program, especially if you have children, are pregnant, or have a disability. You can apply for Medicaid any time of year — Medicaid and CHIP do not have Open Enrollment Periods.
How do I apply for Medicaid and CHIP?
1. Fill out an application through the Health Insurance Marketplace®.
- If it looks like anyone in your household qualifies for Medicaid or CHIP, they’ll send your information to your state agency and the state agency will contact you about enrollment.
- When you submit your Marketplace application, you’ll also find out if you qualify for an individual insurance plan with savings based on your income instead. Plans may be more affordable than you think.
2. You can also apply directly to your state Medicaid agency.
Medicaid expansion & what it means for you
Whether you qualify for Medicaid coverage depends partly on whether your state has expanded its program. Some states have expanded their Medicaid programs to cover all people with household incomes below a certain level, but others haven’t.
In all states: You can qualify for Medicaid based on income, household size, disability, family status, and other factors. Eligibility rules differ between states.
In states that have expanded Medicaid coverage: You can qualify based on your income alone. If your household income is below 133% of the federal poverty level, you qualify. (Because of the way this is calculated, it turns out to be 138% of the federal poverty level. A few states use a different income limit.)
What to do if your income is low, but your state hasn’t expanded Medicaid
Even if your state hasn’t expanded Medicaid and it looks like your income is below the level to qualify for financial help with a Marketplace plan, you should fill out a Marketplace application. Each state has coverage options that could work for you – particularly if you have children, are pregnant, or have a disability. And when you provide more detailed income information you may fall into the range to save.
What to do if you don’t qualify for Medicaid or Marketplace savings
- You can get care at a nearby community health center. The health care law has expanded funding to community health centers, which provide primary care for millions of Americans. These centers provide services on a sliding scale based on your income. Check how to get low-cost care in your community.
- You may qualify for a “Catastrophic” health plan. If you’re under 30 years old, you can enroll in a “Catastrophic” plan. If you’re 30 or older and want to enroll in a “Catastrophic” plan, you must claim an exemption to qualify. Learn more about Catastrophic plans.
- If your expected yearly income increases so it’s between 100% and 400% of the federal poverty level (FPL), you become eligible for a Marketplace plan with advance payments of the premium tax credit (APTC). If your income increases to above 400% FPL, you may still qualify for savings. You’ll find out for sure when you submit an application. In these cases and if your income is at or below 150% FPL, you may qualify for a Special Enrollment Period that allows you to enroll in a Marketplace plan any time of year. You must contact the Marketplace Call Center within 60 days from the date your income changed. When you call, you’ll need to attest that you:
- Weren’t eligible for Medicaid when you first applied because you live in a state that hasn’t expanded Medicaid
- Weren’t eligible for a Marketplace plan with tax credits when you first applied because your income was too low
- Had an increase in expected yearly income that now qualifies you for a Marketplace plan with tax credits
Applying for Children’s Health Insurance Program (CHIP)
CHIP provides low-cost health coverage to children in families that earn too much money to qualify for Medicaid. In some states, CHIP covers pregnant women. Each state offers CHIP coverage, and works closely with its state Medicaid program.
Each state program has its own rules about who qualifies for CHIP. You can apply right now, any time of year, and find out if you qualify. If you apply for Medicaid coverage to your state agency, you’ll also find out if your children qualify for CHIP. If they qualify, you won’t have to buy an insurance plan to cover them.
2 ways to Apply for CHIP:
- Call 1-800-318-2596 (TTY: 1-855-889-4325).
- Fill out an application through the Health Insurance Marketplace®. If it looks like anyone in your household qualifies for Medicaid or CHIP, they will send your information to your state agency. The state agency will then contact you about enrollment. When you submit your Marketplace application, you’ll also find out if you qualify for an individual insurance plan with savings based on your income instead.
What does CHIP cover?
CHIP benefits are different in each state. But all states provide comprehensive coverage, including:
- Routine check-ups
- Immunizations
- Doctor visits
- Prescriptions
- Dental and vision care
- Inpatient and outpatient hospital care
- Laboratory and X-ray services
- Emergency services
States may provide more CHIP benefits. Check with your state for information about covered services.
How much does CHIP cost?
Routine “well child” doctor and dental visits are free under CHIP. But there may be copayments for other services. Some states charge a monthly premium for CHIP coverage. The costs are different in each state, but you won’t have to pay more than 5% of your family’s income for the year.
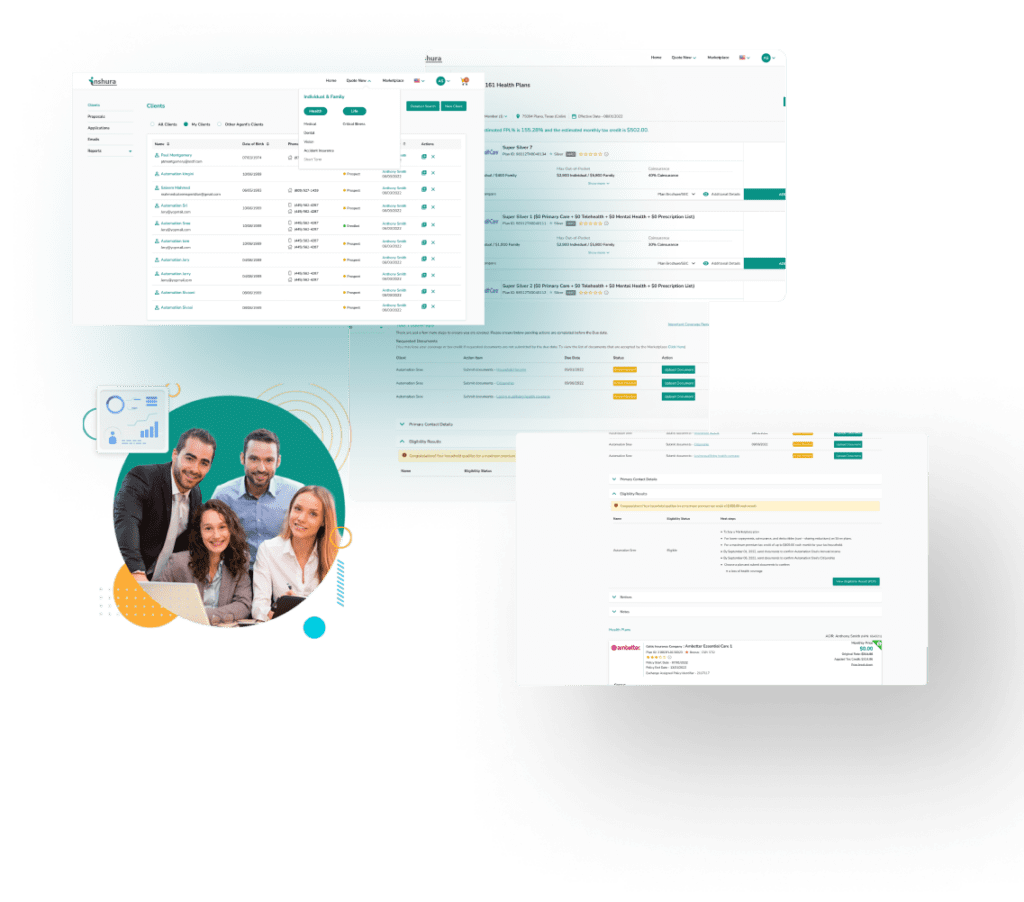
About Inshura
Inshura is a FREE online ACA insurance tool, perfect for agents and agencies! Agents can boost their ACA and other enrollments using this easy-to-use solution for quoting, enrolling, automating renewals, and managing clients!
And inshura is CMS EDE PHASE III certified, so it automatically exchanges data directly from the Marketplace.