Are you navigating the complex world of Medicare compliance? You’re not alone. With numerous guidelines and regulations to follow, it’s essential to have a clear understanding of what is expected from you as a healthcare provider or insurance agent.
In this blog post, we’ll walk you through the do’s and don’ts of Medicare compliance, providing valuable insights on TPMO guidelines, permission to contact, scope of appointment, and events. Whether you’re new to Medicare or looking for a refresher course in compliance best practices, we’ve got you covered. So let’s dive in and ensure that your Medicare operations are running smoothly while staying within the bounds of legality!
Third Party Model Organization Guidelines (TPMO)
TPMO guidelines are an integral part of Medicare compliance. These guidelines outline the expectations and requirements for organizations that work with Medicare beneficiaries.
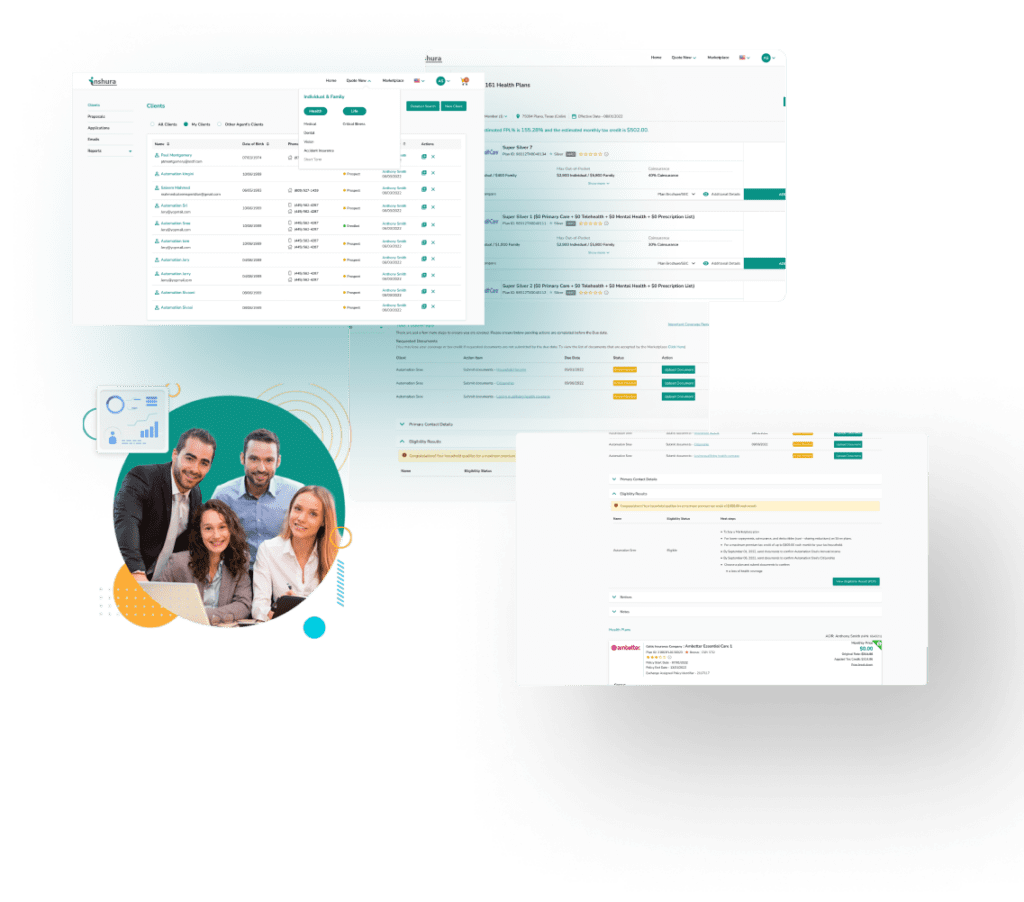
Ensure the privacy and security of patients’ personal health information – It’s crucial to implement robust data protection measures to safeguard sensitive data from unauthorized access or disclosure. Invest in an enrollment platform that’s intelligent and trustworthy, such as Inshura.
Fraud prevention – Providers must have effective systems in place to detect and prevent fraudulent activities related to billing, claims submission, or enrollment processes. This includes regular audits and monitoring procedures to identify any suspicious patterns or discrepancies.
Deliver high-quality care to Medicare beneficiaries – Organizations should strive for continuous improvement in their services by implementing evidence-based practices and adhering to industry standards.
Agents and brokers must record all calls (inbound and outbound calls) in their entirety, including:
- Introductory calls to inform or educate clients about Medicare Advantage and Prescription Drug plans
- Subsequent calls when the beneficiary makes an enrollment decision
- Post-enrollment discussions, including retention-marketing calls that influence a beneficiary’s, to stay enrolled in a current plan
To ensure compliance with TPMO guidelines, it’s essential for healthcare providers and insurance agents to stay updated on any changes or updates issued by the Centers for Medicare & Medicaid Services (CMS). Regular training sessions can help employees understand their responsibilities under these regulations.
Permission to Contact
When it comes to Medicare compliance, one important aspect is obtaining permission to contact potential beneficiaries. This step ensures that agents or brokers can reach out and provide information about available plans without violating any regulations. In the Medicare Advantage & Part D Communication Requirements, agents are permitted to make unsolicited direct contact with potential enrollees via email. However, the email must have an opt-out option in order to remain compliant.
If you use a third-party lead generation company, you must ensure the third-party lead provider understands and follows these requirements on your behalf:
- Disclose to carriers any subcontracted relationships (such as the use of a third-party lead-generation company) used for marketing, lead generation, and enrollment
- Report to carriers, monthly, any staff disciplinary actions associated with beneficiary interaction to the plan
- Disclose to the beneficiary when conducting lead-generating activities that his or her information will be provided to a licensed insurance agent for future contact:
- Verbally when communicating with a beneficiary through the telephone
- In writing when communicating with a beneficiary through mail or other paper communication
- Electronically when communicating with a beneficiary through email, online chat, or other electronic messaging platform
Compliance with permission-to-contact guidelines helps ensure ethical practices are followed when engaging with Medicare beneficiaries. By respecting their privacy rights and seeking consent before contacting them, agents contribute towards building positive relationships based on trust and transparency.
To effectively gain customer trust and follow compliance guidelines, it’s best to use ACA enrollment software that’s EDE Phase III certified by CMS. Inshura.com has an all-in-one platform that efficiently helps you compare, quote, and enroll customers quickly.
Scope of Appointment
Scope of Appointment (SOA) is a crucial concept in Medicare compliance that all agents and brokers must understand. It refers to the specific topics or areas of discussion that can be covered during an appointment with a beneficiary. The SOA ensures that potential enrollees will not be pitched plans other than those they originally requested.
During appointments, it is essential for agents to strictly adhere to the predetermined scope. They should only discuss topics explicitly outlined in the agreement and refrain from veering off-topic. Agents must also ensure they have proper documentation detailing what was covered during each appointment. Per CMS, agents must keep SOA forms on file for at least 10 years, even if the appointment didn’t end in a sale.
What happens if your client requests Medicare information outside of the Scope during your meeting? You must fill out a second Scope covering the new information before continuing the meeting. If they’re interested in non-health related products, you must schedule a future appointment to discuss them.
Failing to adhere to the Scope of Appointment guidelines can result in serious consequences, including penalties and loss of certification as a Medicare agent or broker. It is therefore vital for all professionals operating within this field to prioritize compliance and follow these guidelines diligently.
Events & Appointments
When it comes to Medicare compliance, one of the most important aspects to consider is how you handle events and appointments. These interactions provide valuable opportunities to educate beneficiaries about their options and help them make informed decisions. However, it’s crucial to approach these activities with care and adhere to the rules and regulations set forth by CMS. Here are some Do’s and Don’t’s.
For Educational Events:
DO
- Distribute educational materials free of plan-specific information
- Distribute educational health-care materials
- Give out your business card and contact info for beneficiaries to use to initiate contact
- Collect Scopes of Appointment
- Hold the event in a public venue (optional, but under no circumstance should events be held in-home or in one-on-one settings)
- Schedule future marketing appointments
- Properly document all events and appointments
DON’T
- Distribute plan-specific materials or enrollment packets
- Discuss any carrier-specific plans or benefits or distribute marketing plan materials
- Display a sign-in sheet
For Sales Events:
DO
- Follow the specific carrier’s filing and reporting procedures prior to the event
- Follow the specific carrier’s cancellation procedures
- Make sure to use only carrier-approved materials
- Collect applications
- Call attendees from a sales event if they gave permission for a follow-up call (you must document permission to contact)
DON’T
- Offer meals
- Make absolute statements
- Use pressure to sign someone up
- Cross-sell or promote non-health-related products
- Require attendees to sign in (sign-in sheets MUST be optional)
Final Thoughts
Medicare compliance is an ongoing commitment for those involved in assisting individuals with their healthcare choices. By following TPMO guidelines, such as obtaining permission before contacting potential clients and ensuring adherence to properly documenting educational events, we can contribute towards creating a trustworthy environment. As a result, beneficiaries will feel confident in making informed decisions regarding their health coverage.
Remember – always stay up-to-date with current regulations set forth by CMS; this will not only protect you and your clients but also maintain the integrity of the Medicare system as a whole.
About Inshura
Inshura is a FREE online ACA insurance tool, perfect for agents and agencies! Agents can boost their ACA and other enrollments using this easy-to-use solution for quoting, enrolling, automating renewals, and managing clients!
And inshura is CMS EDE PHASE III certified, so it automatically exchanges data directly from the Marketplace.