The Affordable Care Act (ACA) led to the establishment of the Health Insurance Marketplace where anyone could buy their own health insurance plan. The tax credits created by the ACA meant that Obamacare could be an affordable way to get coverage if you didn’t have employer-based coverage or other health insurance options.
However, the tax credits for these Marketplace plans are only an option when other affordable coverage isn’t available. And according to the ACA, a job-based health plan covering only the employee is affordable if it costs 9.61% or less of the employee’s household income.
If a job-based plan available to an individual is deemed affordable by ACA standards and also meets the law’s “minimum value” standard, then that person and their family are not eligible for a premium tax credit if they choose to buy Marketplace coverage instead. Even if the premiums for an entire family don’t meet that same affordability threshold. As a result, affordable Obamacare coverage may not be affordable at all and the. And the issue of the “Family Glitch” is born.
What is the “Family Glitch”?
Affordability is determined by the lowest priced “self-only” plan that the employer offers – meaning no dependent coverage. The standard for calculating affordability is used solely for the employee, not the whole family—even though the dependents may need to be covered on that same plan.
How does the ACA define affordability?
An employee may have affordable employer-sponsored insurance for herself, spouse and child premiums may be very expensive. Since the employee’s premium is technically affordable, her spouse and children will not be eligible for ACA subsidies.
Many plans that legally qualify as affordable may not be practical nor economical for many families. As a result, these families cannot access premium tax credits for expensive Marketplace plans. Yes, the very tax credits that make Obamacare Marketplace coverage affordable.
Employer-sponsored insurance coverage applies to employees and their children, NOT spouses
After the passage of the ACA, companies with more than 50 employees had to offer health insurance coverage to all employees and their children. But this same affordable coverage rule does not apply to spouses. It’s important to remember that large employers legally must offer coverage for an employee’s dependents. However, the employer doesn’t have to pay for that coverage in the same way they do for the employee’s own coverage.
There is one important distinction, though. If an employee’s spouse isn’t offered health plan coverage, the spouse is still eligible for premium tax credits for Marketplace coverage. This is because technically, no other coverage is available to them. In this scenario, children still would not be able to be eligible for any tax credit for an Obamacare plan. And this is true of children’s coverage regardless of what that coverage costs through the employer.
Who is impacted by the Family Glitch?
Families with low incomes are disproportionately impacted by the family glitch, with estimates putting the number between two and six million Americans. Health insurance coverage is much more costly for workers in the lowest 25 percent of wage categories. In addition, these lowest-earning workers often receive less generous compensation, including a lower percentage of their employer-provided health insurance premiums.
In comparison, those workers in the highest 25 percent of earners in the U.S.pay on average only 30% of their monthly premium costs for job-based health insurance. That translates to about $4,980 annually. Yet workers in the lowest 25 percent of earners in the U.S. pay on average 44 percent of their monthly premium costs for job-based health insurance. And for this demographic, this means $6,324 annually.
Options for Impacted Families
Many families impacted by the family glitch are left with few truly affordable health care options. As a result, many of these families often remain uninsured.
If you’re impacted by the family glitch, your first step should be to check to see if you or your dependents qualify for Medicaid or Children’s Health Insurance Program (CHIP).
Medicaid
Medicaid is a government-funded health insurance program for low-income people. It provides free or low-cost health coverage for eligible low-income adults, children, pregnant women, seniors, and people with disabilities. It is jointly funded by the federal government and the states, and is administered by each state’s Medicaid agency.
Medicaid programs and eligibility vary from state to state. However, 32 states and the District of Columbia, however, have expanded their Medicaid programs. This means that in these places, all people within 138 percent of the Federal Poverty Level can access Medicaid coverage. And this is true regardless of other eligibility factors.
You can apply to see if you or anyone in your family might qualify for Medicaid at any time. Medicaid enrollment is ongoing year-round. This means that you don’t have to wait for the annual Open Enrollment Period for the Marketplace to apply. And you also don’t need to qualify for a Special Enrollment Period in order to apply either.
Children’s Health Insurance Program (CHIP)
The Children’s Health Insurance Program (CHIP) became federal law in 1997. Each state administers their own program, but all CHIP programs have a big similarity. They all exist to help ensure coverage for children in certain types of low-income families. This is a program for kids whose parents still make too much to qualify for Medicaid, but would otherwise be unable to afford health insurance.
The majority of CHIP programs cover children in families with combined household incomes up to 200% of the Federal Poverty Level. CHIP is available to all eligible children ages 19 and younger in families with qualifying incomes. Like with Medicaid, you can apply at any time. You do not have to wait for Open Enrollment. And you do not have to qualify for a Special Enrollment Period. You can apply to see if your child may qualify for CHIP coverage at any time.
CHIP programs vary by state, however, all CHIP programs must cover some basic needs. All CHIP plans cover:
- Routine check-ups
- Immunizations
- Primary care visits
- Prescriptions
- Dental
- Vision
- In-patient and out-patient hospital care
- Emergency services (ambulances and emergency room coverage)
In addition, all preventive care, including annual “well child” exams and immunizations, is completely free for CHIP beneficiaries.
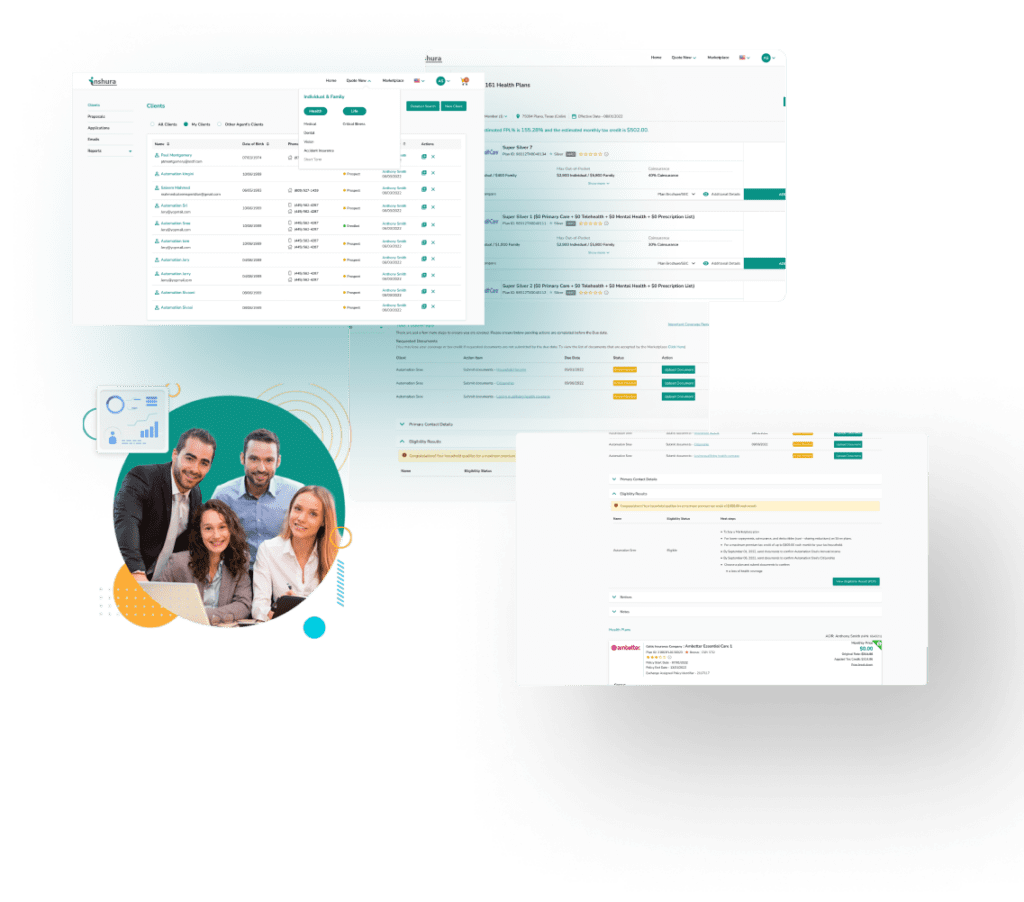
About Inshura
Inshura is a FREE online ACA insurance tool, perfect for agents and agencies! Agents can boost their ACA and other enrollments using this easy-to-use solution for quoting, enrolling, automating renewals, and managing clients!
And inshura is CMS EDE PHASE III certified, so it automatically exchanges data directly from the Marketplace.